Jun 18, 2014 etc
Was a young Waikato midwife at fault in the tragic death of Casey Nathan and her baby?
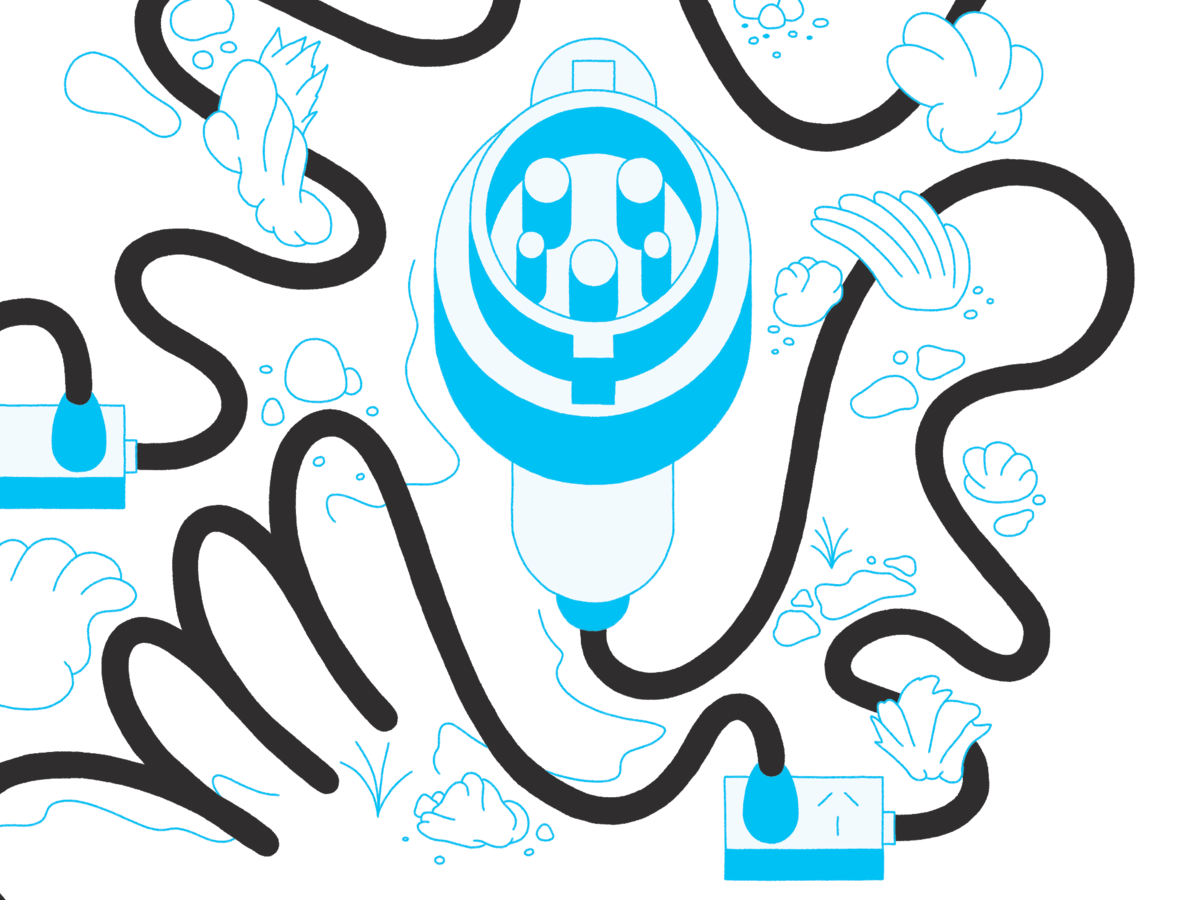
Above: Casey Nathan and partner Hayden Tukiri watch in anguish as midwives try to resuscitate their newborn son, Kymani. Nathan died a few hours later.
First published in the April 2014 issue of Metro. All photos supplied by family.
This is where it ended. On the operating table at Waikato Hospital at 3.26pm on a Monday in autumn, Casey Nathan’s heart stopped beating.
She’d been pumped full of blood, injected with adrenalin and fluid, had her abdomen opened, and her aorta clamped.
There had been, said obstetric anaesthetic consultant Dr Aidan O’Donnell, “this tide of blood coming forth”, from her lungs. It was overwhelming and unstoppable. “We were losing Casey. We’d done everything we could think of, but she was getting worse. I was saying to my colleagues, ‘What do you think we should do? What do you think we should do? What are we missing?’ I was willing to entertain any option at that point to try to save Casey’s life.”
There were 14 doctors and nurses in theatre that day, but neither Casey Nathan nor Kymani, the son she’d given birth to a little over four hours earlier, could be saved. By then it was way too late for high-tech heroics.
This is where it began. At a midwife’s clinic in Huntly on November 3, 2011, where, according to the consultation notes, Nathan was a “well, healthy woman happily expecting her first baby. Lovely strong heartbeat heard today.” And yet, six months later, both mother and baby were dead.
They call it the “Swiss cheese” model of human error in healthcare — the series of minor and, at the time, unremarkable, mistakes that cumulatively, break down the defences of any system so that disaster ensues. There were many holes in Casey Nathan’s care.
Nearly two years on, an inquest over eight days in Hamilton in February heard evidence of a string of failures. By the time she suffered a rare and lethal complication near the end of her labour, some specialists believed, she was already doomed.
The court heard how Nathan’s midwife — despite being in only her first 18 months of practice — used her own judgment to justify setting aside established guidelines for consultation or referral and failed to take basic monitoring tests at several crucial points.
The case, so soon after the 2009 death of baby Adam Barlow after shortcomings in the care of another inexperienced Waikato midwife, could trigger yet more calls for midwifery training to include a mandatory final year in a hospital obstetric unit for midwives planning to practise on their own as lead maternity carers. The coroner, Garry Evans, has made the recommendation before and repeatedly asked witnesses in this hearing what they thought of such an internship.
We can’t tell you the midwife’s name or where she is practising now, because of interim suppression orders. But we can tell you that in her videolink testimony the young woman, despite once breaking down in tears, was confident and articulate. A more senior midwife and former practice partner told the court she had been an “exceptional student” who was “clinically excellent”.
In her testimony, however, she seemed unwilling to accept she might have been too inexperienced to handle the unfolding emergency.
“Do you now accept that you were out of your depth in dealing with what happened that day?” Hamilton Queen’s Counsel Chris Gudsell, assisting the coroner, asked her.
“‘Out of your depth’,” she replied, “is a very broad term.”
Amniotic fluid is like soup. It contains cells, hair, urine from the baby, secretions from the baby. When it enters the maternal bloodstream it seems to be poisonous.
You’ve probably never heard of the complication that killed Casey Nathan on May 21, 2012, and left her son so badly brain damaged he died two days later. It’s called an amniotic fluid embolism and it happens about once in every 13,000-50,000 births, with a fatality rate of around 16 per cent. It’s a feared and poorly understood condition and in New Zealand it kills about two mothers a year.
Doctors don’t know why it happens, except that it’s associated with older mothers, caesarean births, multiple pregnancies and induced labour — none of which applied to Casey Nathan. What they do know is that it happens when the amniotic fluid surrounding the developing baby somehow enters the mother’s bloodstream.
“Amniotic fluid is not water. It’s like soup,” Aidan O’Donnell told the coroner. “It contains cells, hair, urine from the baby, secretions from the baby. When it enters the maternal bloodstream it seems to be extremely poisonous… amazingly poisonous… and it activates a series of inflammatory mechanisms in the mother which are catastrophic and can lead to immediate heart failure, coagulation problems and usually collapse.”
In 16 years, this was the first case of its kind O’Donnell had seen, so it’s understandable that a midwife just 18 months into solo practice had never come across it and failed to recognise its subtle but sinister onset.
Even in retrospect, the only obvious signal something was seriously wrong came around 10.35am, when Nathan lost consciousness for about 30 seconds in the birthing pool at Huntly Birthcare. After that, the midwife was unable to detect a fetal heartbeat and when Kymani was born less than 30 minutes later, he could not breathe on his own and had to be resuscitated.
But there were hints that all was not well with Nathan’s pregnancy much earlier than this. If they’d been acted on differently, the court heard, she could have been referred for obstetric help and delivery in a hospital — rather than at a rural primary birthing unit, 30 minutes away from specialised help.
Nathan did have a single risk factor for amniotic fluid embolism, and that was another condition you probably won’t have heard of — polyhydramnios, an excess of amniotic fluid. It gave her an abnormally large uterus, and it was never diagnosed because the young lead maternity carer (LMC) — the midwife — and one of her colleagues believed the size of the uterus was due to Nathan having a big baby.
She wasn’t. Kymani weighed just 3160 grams (less than seven pounds) and was small. He was born with a congenital malformation of his oesophagus (gullet), known as oesophageal atresia, which means the oesophagus connects to a blind pouch rather than to the stomach. He couldn’t swallow amniotic fluid the way normal babies do. Polyhydramnios is always present to some degree when a baby has that condition.

At the first consultation, on November 3, 2011, the young midwife made her first error of judgment.
Nathan had just turned 20 and was nearly 12 weeks pregnant at that visit. She told the midwife she smoked 8-10 cigarettes a day, was 170cm tall and weighed 75kg — vital information which formed the baseline measurements for her customised “grow chart” that would record how the pregnancy was progressing. Information that, astoundingly, the midwife didn’t check for herself.
“The New Zealand midwifery context is one based on mutual respect and trust and I trusted that Ms Nathan’s reported weight was correct,” she told the court.
With Casey Nathan’s weight at post mortem 99kg and height 166cm, the midwife conceded that she had probably weighed more than 75kg at that first appointment. From then on, the “customised” chart was intrinsically flawed. The midwife told the inquest she no longer takes a mother’s word about her weight and height.
Soon after that first visit came signs that Nathan’s antenatal care might not be straightforward. In a report to the coroner, the midwife said visits were rushed because Nathan’s partner, Hayden Tukiri, had a “limited attention span” and they both wanted to leave before the end, so appointments were 10-15 minutes shorter than normal. Colleague Sheryl Wright, who tracked Nathan to a cousin’s home while the lead midwife was on holiday, told how she’d been terrified when a dog was released and lunged at her and how she suspected Tukiri was on drugs.
By March, measurements showed that Nathan’s uterus was bigger than it should have been and, suspecting diabetes, the LMC sent her for a glucose tolerance test. After that, if the test was positive, she was to have an ultrasound scan. It was negative and no scan was done.
In the last trimester of her pregnancy, Nathan failed to show up for four antenatal visits, and the court heard how hard the midwives tried to locate her and ensure she was seen — often phoning and texting repeatedly and visiting a number of houses where they thought she might be. By the end of her pregnancy, three midwives had measured her belly size, a factor which they said could also make measurements variable and less reliable.
The last reading — taken by a backup midwife, Nicky Mecchia, on the Friday before Nathan gave birth the following Monday — was so high the chart recommended a scan but, because of the timing, it would have had to have been an urgent weekend referral and Mecchia didn’t think that was justified. “I did briefly think about a scan but I didn’t think it would be practicable.”
As coroner Evans asked one of the three midwives: “What is the point of doing these charts if nothing happens?”
So despite the worrying readings showing that either her baby was very large or something else was causing her uterus to be abnormally big, by the time Casey Nathan was admitted to Huntly Birthcare at 1am on May 21, neither the midwives nor the patient were aware this might be anything other than a straightforward labour in a healthy young woman.
At the coroner’s inquest, Auckland obstetrician Dr Tony Baird pointed to a string of factors he believed should have alerted the midwives to the need for an obstetric consultation. “Faced with a first young mum, smoking, Maori, overweight… when she became clearly large for dates, I would have expected a consultation.”
While Baird said that would have been justified during her pregnancy, there were also missed opportunities for referral during her labour — especially at the early stage when dilation of her cervix was slow and guidelines recommended an obstetric consultation. But the young lead midwife says she didn’t seek that consultation because she believed there had been progress in other ways, including that the baby had descended, its head was in a better position for the birth and the overall labour was not prolonged.
Nathan had been in the warm birthing pool for a short period a little after 3am, and wanted to return to it six hours later. The midwife, worried that it might slow her contractions, tried to prevent this. She failed. “The whanau were irritated that I was not going to let her back into the pool as many of their family members had birthed in the pool and found it to be helpful for pain relief. I agreed on the condition that we monitor progress.”
Nathan collapsed in the pool an hour later, at 10.35am.
The midwife admitted that, while she’d taken the fetal heart rate, she hadn’t taken Nathan’s blood pressure or heart readings before her collapse. When she did try to take them after it, Tukiri became “vocal and abusive”, according to Huntly Birthcare manager Korina Vaughn, who’d been called in to assist.
The midwife told the hearing she should have askfed for a “status one” ambulance but didn’t know the St John coding had changed.
While Nathan appeared to recover quickly from what the midwives present called “a faint”, the lead midwife recognised the seriousness and rarity of the collapse and called 111 for a “priority one” ambulance. She believed she was summoning a crew of two paramedics.
The inquest heard, however, that her description of Nathan’s condition as a woman in labour who’d fainted in the birthing pool didn’t convey its seriousness and St John sent the only vehicle available in accordance with a “priority one” call — an ambulance staffed by one woman with no advanced paramedic training.
The midwife told the hearing she should have asked for a “status one” ambulance but didn’t know the St John coding had changed.
Though they considered transferring Nathan to hospital immediately, the birth appeared imminent, so they decided to break Nathan’s waters and get Kymani out. “We needed to get this baby delivered,” Vaughn said.
After the birth, at 11.02am, with the mother appearing well — but without the reassurance of respiratory and blood pressure readings to back this up — the attention of the three midwives and a Huntly Birthcare nurse turned to the baby, born pale and limp and unable to breathe on his own. “I understand the initial panic,” said one witness, “but it appears this panic may have continued.”
Though an ambulance was by now on site, Waikato Hospital’s neonatal intensive care retrieval team — two neonatal nurses in an ambulance — were summoned. It arrived at 12.15pm.
Five minutes later, when the young midwife finally took Nathan’s readings — measurements which by now hadn’t been taken for more than four hours — she realised she, too, was in serious trouble, with low blood pressure and a high pulse rate. At 12.55pm, the neonatal nurses allowed Casey Nathan to kiss her baby before they took him to Waikato Hospital. It was to be the only time after the birth that they touched.
The next time they were together was in a coffin at their combined tangi.
Casey Nathan left in the second ambulance at 1.08pm, together with Tukiri and the midwife. Her condition deteriorated rapidly. By the time paramedics sent from Hamilton met the ambulance between Ngaruawahia and Horotiu, she was, said paramedic Nigel Dawson, “as close to death as you can possibly be and still being alive, in my experience.”
Her blood pressure was so low it was unrecordable. “She was pale, she was clammy, she was very, very restless. She obviously had hypoxia [lack of oxygen], her heart rate was high.”
“Babe,” Nathan told Tukiri, “I’m gonna die.”
She was pale, she was clammy, she was restless, her heart rate was high. “Babe,” she told him, “I’m gonna die.”
Within two minutes of arriving at Waikato Hospital at 1.58pm, Nathan was wheeled into theatre. Her last words were a brief medical history whispered through an oxygen mask to O’Donnell, bent low to her ear.
The operating team, believing the most likely explanation for her critical state was a massive haemorrhage, began pumping blood into Nathan. “If haemorrhage were the only problem with Casey, we would have expected to see her improve rapidly,” O’Donnell told the inquest. “Instead, she improved only marginally. At first I thought, ‘Oh yeah, we’re winning,’” he said, but then Nathan’s condition plateaued. “That was the first thing that made me think, maybe there’s something else going on here.”
They opened Nathan’s abdomen, thinking she was haemorrhaging internally and were “astonished” to find she was not. “We couldn’t account for why Casey wasn’t improving. We started to consider alternative diagnoses. What else could this be?”
At this point, Nathan’s ECG readings began changing, showing her heart had begun to “really struggle” and O’Donnell began to suspect an amniotic fetal embolism.
“We’d done everything we could think of. We’d given her blood. We’d given her adrenaline. We’d given her fluid and she wasn’t getting better. In fact, she was getting worse.”
As her blood pressure dropped, “it was plain she was going to arrest”. At 3pm, Nathan’s heart stopped. The team shocked her back into life with a defibrillator.
“That first arrest was a big step downwards. After that she was worse in almost every way. Blood started to come up her breathing tube, so somewhere in her chest there was blood and it was gushing, surging up the endotracheal tube. And once that blood started to come up it became impossible for us to get any oxygen back down, we couldn’t get the oxygen into her lungs anymore.”
At 3.15pm, O’Donnell says he realised their efforts were futile but, because of her age and prior good health, they kept trying. Two surgeons reopened her abdomen and clamped her aorta in a last, desperate bid to save her life. That, too, failed and the team stopped all resuscitation at 3.25pm. Nathan’s heart stopped beating a minute later. It had been, coroner Evans remarked, “a Herculean effort to try to save poor Ms Nathan’s life”.
O’Donnell told the inquest that while Nathan’s chances would have been better had she come to hospital earlier, he couldn’t say by how much.
“I regard amniotic fluid embolism syndrome as being like a bush fire. Once it has taken hold, you can’t treat it, there’s nothing you can give to make it better, you can only attempt to keep the flames out and prevent it from spreading but even in that circumstance that’s not always possible. So even if Casey was in our care [for the birth], in our delivery suite and we suspected that she had an amniotic fluid embolism, we may not have been able to turn this around.”
He said the midwives had recognised the faint was abnormal and had done the right thing by calling for help immediately. “I see that they are doing it in a circumstance of extreme urgency where the life of the baby is under threat, where there are two ambulance teams and there’s a great deal of fear and terror and people trying to do the very best that they can in a situation which was clearly spiralling out of control quite rapidly.”
 The coroner has reserved his decision. While it’s possible Nathan might not have survived the embolism wherever she gave birth, among the key questions he will consider is whether she was a proper candidate to have her baby in a low-tech primary birthing unit at all — given the measurements suggesting she had an abnormally large uterus or baby — or whether she should have been transferred hours earlier, when her labour was not progressing well.
The coroner has reserved his decision. While it’s possible Nathan might not have survived the embolism wherever she gave birth, among the key questions he will consider is whether she was a proper candidate to have her baby in a low-tech primary birthing unit at all — given the measurements suggesting she had an abnormally large uterus or baby — or whether she should have been transferred hours earlier, when her labour was not progressing well.
College of Midwives midwifery standards reviewer Stephanie Vague, in a report for the coroner, said she believed the midwifery care Nathan received, both antenatally and during her labour and birth, was “appropriate under the circumstances”.
A second expert witness nominated by the College of Midwives, Jacqui Anderson, said she wasn’t convinced Nathan had severe polyhydramnios because three midwives had missed it, and felt they could readily palpate the baby. “It’s very unusual to miss that.” But she accepted that because of Kymani’s congenital malformation, the condition had to be there to some degree.
But even putting that condition aside, should Casey Nathan have been giving birth at the Huntly unit with no immediate medical back-up and an inexperienced midwife?
Recently retired Canterbury midwife Margaret McGowan told the coroner there were a raft of reasons she shouldn’t have delivered there, including the fact she was a smoker, hadn’t turned up for all visits, had a low socio-economic status, was thought to be having a large baby and it was her first birth.
Auckland obstetrician Sylvia Rosevear agreed. “I have been reliably informed by midwives in Auckland that they would not consider a smoker low risk. Full stop.” But another obstetrician, John Tait, of Wellington’s Capital and Coast District Health Board said, “I don’t think you can make every person who smokes deliver in a secondary or tertiary hospital. I think we’ve got too many smokers for that.”
He believed with three midwives deeming her able to give birth in Huntly, “my own view would be that it would be fine to start off there, but there are a number of red flags that would make you transfer possibly earlier rather than later”.
Had the transfer happened at 7am, 8am or 9am, Tait said, before the embolism occurred, it was a “real possibility” an obstetrician at Waikato Hospital would have immediately broken her waters — and the embolism, which happens only when the waters are intact, would have been avoided.
The inquest didn’t hear directly from Casey Nathan’s partner Hayden Tukiri, or their whanau, but Action to Improve Maternity spokeswoman Jenn Hooper, who’s been supporting the family since the deaths, said they felt “lighter and calmer” after listening to the minute-by-minute accounts of what happened to Nathan and Kymani. “They feel they have the answers to what happened.”
The AIM group, which supports families who have lost children or had children born with disabilities when births went wrong, says common “red flag indicators” of problems keep cropping up — including in this case. They included lack of monitoring during late pregnancy and labour, the lead maternity carer “normalising the abnormal”, a failure to progress in labour, poor documentation and lack of action when warning signs appeared.
While Casey Nathan hadn’t turned up to some antenatal visits, “she’s a 20-year-old extra-heavily pregnant girl in winter in Huntly with no car”. She says young women, many of whom were at higher risk of complications, often chose young midwives because they believed they would get on better with them.
“I often start these cases with a bit of sympathy for the practitioner — she’s got to live with this for the rest of her days. I start losing that sympathy when the facts come in.”