Mar 1, 2017 etc
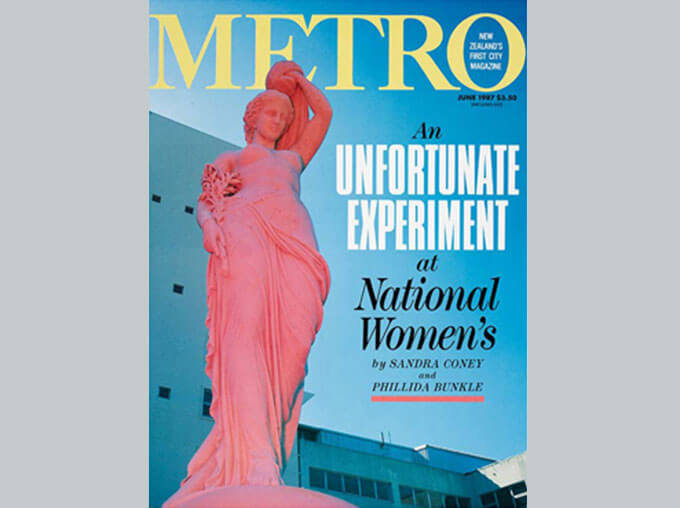
Read the original Metro article, published in June 1987, that exposed the practices of doctors at New Zealand’s leading women’s hospital. The article by Sandra Coney and Phillida Bunkle led to a Commission of Inquiry, headed by Dame Silvia Cartwright, that helped strengthen patients’ rights and saw the establishment of a national cervical screening programme.
In October 1985, Ruth (not her real name for legal reasons that will become clear later in this story) returned from National Women’s Hospital and told her workmates she felt she’d just been to Auschwitz. “I feel as if they’ve been experimenting on me, she said. Ruth’s fellow teachers thought she was being ridiculous and said so and so she pushed her doubts to the back of her mind.
It was over 20 years since Ruth had made her first visit to National Women’s Hospital. She had not been a teacher then, but a 27-year-old suburban mother of three small children. She had failed UE and with “the disadvantage of no education” remembers herself as the “the sort of patient who meekly did what she was told.”
She had been referred to the hospital by her general practitioner after a “suspicious cervical smear. Having a cervical smear means that cell are collected from the surface of the neck of the womb using a sort of ice block stick, then smeared in a thin film across a glass plate so that their structure can be seen through a microscope.
At the hospital Ruth was told that though her smear was “suspicious”, nothing more serious was going on. She came home and reassured her husband that she didn’t have cancer and that there was nothing to worry about. “That”, she remembers, “was the frame of mind they put me in from the beginning.”
Six months later she had an examination of her cervix with the colposcope, a powerful magnifying instrument and a single punch biopsy removed a fragment of tissue the size of a rice grain for scrutiny in the pathology laboratory. In the space of the next six months, Ruth bad three colposcopies and three smears were taken. She felt confident that she was being carefully watched.
In mid-1965, Ruth became pregnant. Her GP was surprised when she told him about the pregnancy. “What do they think at National Women’s?” he asked. Ruth told him the doctor she saw at the hospital said it was fine and her GP agreed that he must know what he was doing. In March 1966, Ruth gave birth to her fourth child, a healthy eight pound girl.

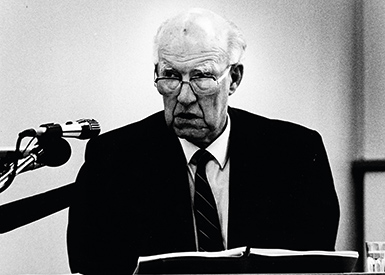
Herb Green was an expert on cervical cancer. He was on the world circuit, attending conferences and publishing frequently on the subject in prestigious gynaecological journals. From 1956 to 1982 when he retired, he saw virtually every woman at National Women’s Hospital with invasive cervical cancer and many of the women who had earlier or “precursor” stages, a total of some 1800 women.
Professor Green became a man with a mission. He wanted to save women from mutilating surgery and to do so he had to prove what at first he had suspected and eventually came to believe: that CIS was a harmless disease which hardly, if ever, progressed to invasive cancer.
Green was born in Balclutha in 1916. He qualified from Otago Medical School in 1945, where he had won his rugby blue. A Southland representative cricket player, he was a powerfully built man who towered over his colleagues. In 1948 he took a position as a house surgeon at National Women’s Hospital in Auckland. He immediately became involved in the treatment of cervical cancer.
National Women’s was in its infancy. It had opened in 1946 to provide for the post-war baby boom. The powerful Obstetric and Gynaecological Society, wishing to consolidate its power by controlling the teaching of obstetrics and gynaecology, pushed for the establishment of a post-graduate school based at National Women’s. With the support of the Auckland business community, it endowed a professorial chair. An Australia, Harvey Carey, took over the position in 1954. Carey was liberal in his views, and would ultimately fall foul of the obstetricians by advocating less medical interference in childbirth and opposing a specialist monopoly of the planned unit. Carey was also keen to test the use of cytology in the detection of cervical cancer.
National Women’s Hospital had inherited responsibility for the treatment of cervical cancer from Ward 4 at Auckland Hospital. It took cases from the whole of the northern half of the North Island and by 1954 a specialised clinical team had been set up.
Invasive cervical cancer is described as “the most miserable of cancers”. In the days before cytology it was not always detectable until at an advanced stage when there would be the unusual bleeding from the uterus or a visible growth on the cervix. The only treatment was by deep ray or radium, although in the early 1950s surgery was introduced at National Women’s as an additional treatment. Invasive cancer was thought to go through earlier or “precursor stages”. These stages were called dysplasia, or abnormal cells, the most abnormal cell being carcinoma in situ, or CIS (pronounced kiss). CIS was believed to finally process to invasive cancer.
A smear from the cervix might reveal cell changes in the earlier stages. The theory was that if cancer could be detected before it reached the advanced invasive stage, it might be possible to remove it and cure the disease.
Carey knew that at nearby Greenlane Hospital Dr Stephen Williams’ cytological smear tests of sputum had been successful in detecting an unsuspected lung cancer.
He knew that too in New York, Dr Papaniculoau, inventor of the “Pap Smear” was “booming away about his cause”. Carey went to Williams, and as Williams recalls, begged him to do a trial run of 1000 cervical smears of women entering the hospital for other causes. “Of course”, he remembers, “long before we had done 1000, at about the two hundreth specimen, we had turned up an extraordinary smear of carcinoma in situ with cancer cells spread right across the smear. There had been not the slightest sign of cancer on her cervix. Carey was dumbfounded. We did a biopsy tissue test of the cervix and discovered loads of CIS in the tissue.”
With this success, the programme did not stop at 1000 smears. It continued and a full-time cytologist was appointed to National Women’s to set up a laboratory to train staff. He was sent to the United States to study cytology at first hand, and on his return the Papaniculoau grading sequence was introduced. By 1957 the “Pap Smear” was offered to all doctors in New Zealand.
Carey was evangelistic in his belief of the benefits of screening. Remembers Williams: “Carey raced around like a bee in a fit. He wrote an article for the Women’s Weekly saying that cervical screening could save lives. He concluded that he could save five lives for every 1000 smears, a wildly exaggerated claim as it turned out.”
By 1964 the hospital cytology service was seeing 20,000 specimens a year. The year before, National Women’s had shifted from its original Cornwall Hospital premises to a new $3 million purpose-built premises in Claude Road, Epsom.
It also had a new head, Londoner Dennis Bonham, elevated to status of professor from a position of lecturer at University College Hospital, London.
A new cytology block was put out to tender in 1964, but by this time Herb Green had stepped in and said he was having doubts.
Green had joined the cervical cancer clinical team in 1955. He and another colleague had done a limited number of smears in 1948, but he had been out of the country when the major initiatives on cervical cancer were taken.
Green wasn’t convinced of the idea of progression of the disease, that carcinoma in situ developed into the potentially fatal invasive cancer. He argued that invasive cancer was probably a quite separate disease. His theory was that if there was little or no progression, then CIS was not a harmful disease and screening for cervical abnomalities would not lead to a reduction in the incidence of invasive cancer. This was the position he would express for the next two decades.
When Ruth first visited National Women’s in August 1964, she had no idea that there was any debate about cervical cancer or that her doctor held controversial views. She was quite sure she was in the best of hands. She was put on the waiting list for a cone biopsy, an operation which removed a cone-shaped core at the cervix which could be checked to see that all abnormal tissue had been taken.
But the day following her admission for the cone biopsy, after preparations for the operation had been made, Professor Green told her that he had decided against operating and she was discharged without any treatment.
Every few months after this Ruth was recalled to the hospital where she had further smears, colposcopic examinations and occasional punch biopsies.
The purpose of a punch biopsy is to diagnose what the disease is and how far it has gone. It enables the pathologist in the lab to scrutinise a small section of the cervix under the microscope, look at the cells and say what they are doing. Very occasionally a punch biopsy can cure CIS, but it is most unlikely as the sample is so minute. It has never been regarded as treatment for cancer.
Treatment involves more extensive surgery to remove the cancerous cells, the object of any treatment being to return to a negative (normal) smear later.
Ruth’s first punch biopsy in 1965 showed a carcinoma in situ, a diagnosis which would be mistakenly entered on her records for 15 years. Her smears were almost invariably positive (abnormal, and the reports described the cells as “suggestive or “strongly suggestive” of malignancy. But this Ruth did not know.
Many years later, in 1985, Ruth would see her hospital file and finally know that from her first visits she already had carcinoma in situ. ln 1964,and over the years, the words were never mentioned.
By May 1967 the colposcopist entered in her notes that he had observed that the abnormal area on Ruth’s cervix had increased in size in the two years since the first colposcopic examination. By the end of that year he recorded “progression both in extent and degree”. Throughout 1968 and 1969 Ruth’s smear reports were “conclusive for malignancy”. But still nothing was done.
In March 1970 Ruth was admitted for a curette of the uterus (a scraping out of the lining of the uterus) and wedge biopsies.
A wedge biopsy takes a rather larger piece of tissue than a punch biopsy but it is also used mainly for diagnosis although rarely it can be a cure. Ruth’s pathology report showed carcinoma in situ in all the specimens and in one “micro-invasion of the cervix”. This is the first sign that the cancer is penetrating deeper layers of cells and becoming invasive.
Despite this, Ruth was again discharged. She returned for smears right through 1970, each one showing cells still “strongly suggestive” or “conclusive for malignancy”.
Ruth still had the disease and still did not know it.

It was experience with young childless women which started Herb Green asking questions about the diagnosis and treatment of cervical cancer.
“When you see a young attractive woman who’d make a wonderful friend for a man a little younger than myself, when you see her die, it’s not nice.
By the early sixties, the idea of the progression of cervical cancer through precursor stages was generally accepted in the medical community. But the disease was not completely understood and there was room for argument. The causes of cervical cancer were not known. How often it progressed and how quickly, was the subject of debate. It was strongly argued that widespread screening programmes would reduce the incidence of cancer by detecting it earlier and the large programme underway in British Columbia, Canada, was being watched with interest.
Women with abnormal smears were customarily investigated further by biopsy to diagnose more accurately the stage of the disease. The standard treatment for the precursor stages was cone biopsy.
Cone biopsy is described as a “nasty operation”. Haemorrhage needing emergency treatment is not an uncommon problem and the woman’s chances of conceiving afterwards can be significantly reduced. The cervix can be so scarred that menstruation can become difficult and very painful.
For carcinoma in situ the standard treatment was hysterectomy, a major operation involving removal of the uterus or womb which therefore rendered the woman sterile.
Twenty-five years later Herb Green can remember in vivid detail some of the cases which distressed him most. A young poet had her university degree conferred in a ceremony in Ward 9 a week before she died of cancer of the cervix. “When you see a young attractive woman who’d make a wonderful friend for a man a little younger than myself, when you see her die, it’s not nice. That’s why I’ve been so vocal. This is bad for mankind. I realised at the time she wasn’t the only one under 30, there were four,” he recalls.
He remembers too another patient who gave him the clue which formed the basis of his theory. He calls her “the little girl who put me on the right track.” Green performed a biopsy disclosing CIS, but the woman “refused a hysterectomy. “Two years later she had a baby. She’s still alive, living somewhere round Whenuapai.”
Green was concerned at any reduction in women’s fertility. He was an opponent of abortion and with his gynaecologist colleagues Patrick Dunn and William Liley, later played a leading role in the early days of the Society for the Protection of the Unborn Child (SPUC). He took such an uncompromising view of abortion, calling it murder, that he was used to present the extreme anti-abortion view to Auckland Medical School students. At one stage he caused a furore at National Women’s by refusing to work with doctors performing abortions.
On sterilisation he also held conservative views. He could see virtually no grounds for it, medical or social, arguing that abstinence would lead to the desired result. Once sterilised, he said, a woman had “thrown away a unique possession”.
Professor Green became a man with a mission. He wanted to save women from mutilating surgery and to do so he had to prove what at first he had suspected and eventually came to believe: that CIS was a harmless disease which hardly, if ever, progressed to invasive cancer.
Green’s belief led him to treat some patients less extensively. He stopped performing routine hysterectomies in women with CIS and instead performed cone biopsies, checking by pathology (tissue diagnosis) that the complete tumour had been removed. Br 1962 he was able to report that no patients treated this way had progressed to invasion.
There was no hospital plan to seek the agreement of the women to their unorthodox management. Thus, like Ruth, they were unaware they were getting anything other than standard management for their disease.
Time had shown that Green was correct in arguing for more limited treatment of CIS patients. Many women were saved from unnecessary hysterectomies, and by the mid-sixties cone biopsy for CIS had become standard treatment.
Having made a breakthrough and having produced what looked like support for his hypothesis, Green pushed the limits of his theory further. Many other medical authors had published papers in the fifties and early sixties estimating that ClS progressed to invasion in a “variable proportion of cases. Green proposed “to show that the lesion is probably benign in the great majority of cases” and to question the view that screening programmes could eliminate invasive cancer.
He began to treat small groups in unorthodox ways. At least five women, and possibly as many as 16, had hysterectomies without prior biopsies to diagnose what was happening to the cervix. Green had only looked at the cervix with the naked eye and taken a Pap smear. A Pap smear can reveal an abnormality, but a biopsy is necessary to accurately say what stage the disease is at. Earlier, Green had always argued that biopsies were vital for proper diagnosis. In these cases he’d omitted this step. One result was to provide him with intact cancer lesions to study in the laboratory.
In Green’s words, these patients formed a “special series wherein invasive cancer has been ruled out as far as possible by clinical [looking and listening to the patients] and cytological methods before hysterectomy; serial section studies of lesions thus undisturbed by biopsy are being made and will be reported separately.”
There were two dangers in performing a hysterectomy without biopsy. First, a healthy uterus might be mistakenly removed. Second, and possibly fatally, if the woman, in fact, has invasive cancer it would be difficult to treat optimally with radiation therapy after a hysterectomy. In this treatment, radioactive rods are inserted through the cervix to sterilise the uterus and adjacent tissue. With the womb removed, the rods could not be put in place.
Because in these cases Green had not done biopsies before surgery, the only way to detect the seriousness of the disease and see if more treatment was needed, was to immediately examine the excised wombs in the pathology laboratory. Before this could be done, Green took some of the wombs with him to New York when he left in 1962 on a year’s Lederle Scholarship.
Two months later, National Women’s received a note from New York. Green was reporting that one of the wombs had shown the woman actually had invasive cancer at the time of her hysterectomy. Despite more extensive surgery, she died two years later.
In other groups of patients the abnormal tissue was not completely removed, or Green “temporised – that is delayed – further treatment, despite positive smears continuing after cone biopsies. This, he acknowledged in writing, “may appear foolhardy to those who believe in a high chance of progression of the disease to invasion”.
Although it is clear from Green’s writing that he knew his was a minority view, and that he was providing unorthodox treatment, he did not think the patient should be the one deciding: “lf we are uncertain about the natural history of the disease which cytology has revealed in her, how can we possibly expect her to make what is really our decision?” he asked.
Green justified his unusual handling of cases by insisting that he always rigorously excluded the possibility of invasive cancer before deciding on limited treatment. He also produced his results in vindication of his methods. For much of the sixties he insisted that not a single case had progressed to invasion.
In April 1963, Green embarked on another study. Between this date and June 1965 the rate of cone biopsy at National Women’s doubled, peaking at 140 operations annually before falling to below 40 in 1966. Wrote Green: “200 [cone biopsies] were performed by the author as a special study”, one of the aims being to ”estimate in a consecutive series” the correlation between the grade of the prior smear with the later histology (tissue diagnosis) report. In nine women, the smears had showed nothing wrong. Their cervices were only coned because they “looked suspicious”.
In fact, the post-operative histology reports showed that five of these women only had cervicitis, a mild inflammation of the cervix in no way requiring such drastic treatment.
By the mid-sixties Green was so convinced CIS was harmless he even argued against the necessity for cone biopsy, a proposition he decided to test by omitting the cone biopsy on some women. This could have been the reason for the cancellation of Ruth’s cone biopsy in 1964.
In June 1966 Green finalised his experiment and gained permission from the Hospital Medical Committee to manage a group of women “conservatively”, that is, to withhold conventional treatment of cone biopsy or hysterectomy. The women selected were under 35 and the possibility of existing invasive cancer was excluded by punch biopsy performed by a colposcopist looking at the magnified cervix.
Colposcopy was introduced to National Women’s in the mid-sixties. The colposcope sharpened the view of the cervix, enabling abnormal cells be seen in a way they could not be by the naked eye. The site for biopsies could then be carefully chosen, rather than the more random method of the past.
In the women Green managed “conservatively'”, the lesion was to be damaged as little as possible by the biopsy, and despite continuing abnormal positive smears, the women were to get no further treatment.
Other women who had abnormal smears after initial treatment, such as cone biopsy or hysterectomy, were also to receive no more treatment. According to a paper by Green, by the end of 1966, some 73 women with evidence of persistent, uncured CIS were being followed. Twelve of these had diagnosed microinvasion of the cervix. Sixteen had only a punch biopsy.
Differences of opinion over the best treatment for CIS were one thing but there was always unanimity in the medical community about the object of treatment – to return to a negative or normal smear. A positive smear was a sign that treatment had not been successful, that there was still disease present and there had been no “cure”. In such cases, further treatment was called for, until the smear became normal.
This was never the intention of the National Women’s experiment. Some women with evidence of the disease were to be left. They would be followed – that is, brought back for regular smears and possibly more biopsies, but there was no intention to cure them.
The dangers of this are many. If the initial diagnosis was inaccurate, women might be unwittingly harbouring an advanced stage of the disease. Women might ultimately need unnecessarily extensive treatment to cure invasive disease. They might even die, for once the cancer has become invasive, treatment will not always halt the disease. In addition, if they failed to attend for follow-up, missed appointments or moved overseas they were at serious risk.
But by watching these women, Green hoped to observe the natural history of the disease and prove his thesis, that untreated CIS rarely, if at all, led to invasion.
The words “natural history of the disease” are important and need to be emphasised. “Natural history” means what the disease will do if it is not interfered with by medical treatment. Many overseas researchers interested in cervical cancer would very much have liked to study the natural history of cervical cancer, but it was considered unethical to do so. If you believed in the progression of the disease, as they did, you could not risk women’s developing the potential fatal form but not treating its precursors.
Asked to comment on this study, Leopold Koss, Professor of Pathology at Montefiore Medical Centre and Albert Einstein College of Medicine in the Bronx, New York, the leading world authority on cytology wrote: “..there is excellent evidence that not all of these precancerous lesions progress to cancer, hence a large number of them might be presumed to be unnecessarily treated. Dr Green stresses this point repeatedly in his papers, and as far as this issue is concerned he is completely correct.
“On the other hand, neither he nor anyone else can predict which one of the precancerous lesions will progress to cancer and which will not. Therefore all must be treated.
“Dr Green is a senior and generally respected gynacologist who is a well-known contrarian. I must stress though that the most serious observers of the cervix cancer scene do not agree with his views.”
Dr David Boyes, director of the Cancer Control Agency of British Columbia and author of the studies which have convinced the rest of the world of the efficacy of cancer screening makes a similar comment: “…unless the whole lesion was removed, it was not possible to know whether there was some beginning invasion. We have never considered that it was appropriate in man to study the natural history in this fashion because one never knew what one was dealing with unless the whole lesion was removed.”
Ralph Rickart, Professor in Pathology and chief of the division of Obstetrics and Gynaecology, Pathology and Cytology at Columbia University College in New York, is more forceful. He doesn’t think the study should ever have been started. “By the late fifties, and certainly by the mid-sixties, there was little debate on the fact that CIS progressed. The weight of evidence at the time was that CIS progressed. The weight of evidence at the time was that CIS was a precursor. Others had conducted long-term studies on the disease but had used CIS as an end point. It was absolutely unacceptable and unethical to follow people past that point.”
Rickart believes that most cancer lesions progress if the women live long enough for that to become evident. “At best,” he says. “75% will progress within 10 years.”
There was debate about progression in the sixties but the debate in the rest of the world was about the progression rate, not whether it did or did not progress.
In one of his papers, Green quotes the famous New Zealand gynaecological specialist, Professor Stallworthy, Professor of Obstetrics and Gynaecology at Oxford University as having said in 1966: “To regard carcinoma in situ as not being a killing disease is comparable to giving a stiletto to a paranoiac.”
In another paper Green quotes the opinions about progression held by others at this time: Dunne et al (1959) 100% progression rate, Lange (1960) 33.3% progression rate; Boyes et al (1962) 60%, Graham et al (1962) 10·20%, McGregor and Baird (1963) 33.3%, McGregor (1966), 100%.
These figures are quoted to show that Green was out on a limb. His opinion was not shared by the medical community and he knew it. A 1970 paper in an Australasian medical journal was headed An Atypical View. In it Green said that by “commonly accepted standards many in-situ lesions have been almost disdainfully under-treated”, and that “It is clear that the author’s experience with cervical carcinoma in situ is at considerable variance with that of the great majority of others.” He called others’ belief in progression a “dogma” which had become ”immutable and almost unchallengeable” and so he set about challenging it.
Professor Green described the purpose of the experiment this way: “The only way to settle finally me problems of what happens to in situ cancer is to follow indefinitely patients with diagnosed but untreated lesions. This is being attempted.”
Discussion of the ethics of the study never appeared in his papers, perhaps because he believed so absolutely that women with CIS would not develop invasive cancer Green has written: “If the physician does not worry too much about the disease then neither will the patient.”
Consequently, patients like Ruth did not know they were being studied, nor that they were being treated in an unorthodox way. In his paper The Natural History Of Cervical Carcinoma In Situ Green described the arbitrary manner in which women were selected. “No clear pattern of selection is discernible, and subsequent treatment was most often a matter of chance, dependent on the views of the consultant under whom the patient was admitted – and, therefore, really on what day of the week the patient was referred to the clinic.”
It has been impossible to discover whether all the patients given limited treatment were Herb Green’s. Neither the present medical superintendent of the hospital, Dr Gabrielle Collision, nor the head of the postgraduate school both then and now, Professor Dennis Bonham, could answer this question, although Bonham said other doctors referred CIS cases to Green “because of his interest”.
In answer to a question about whether women were told there were differences of opinion about the methods of treatment, Green replied: “I suppose not.”
In answer to the same question, Professor Bonham said: “I wouldn’t know, you would have to ask each individual doctor who treated patients.”
There was no hospital plan to seek the agreement of the women to their unorthodox management. Thus, like Ruth, they were unaware they were getting anything other than standard management for their disease.
In 1966 there was no ethics committee in the hospital. At that date, no hospital in New Zealand had one. The study was passed by the Hospital Medical Committee of which Bonham was chairman.
But despite the lack of an ethics committee, international standards for human experimentation did exist.
Ethical standards for human experimentation had been set by the Nuremberg Code in 1947. The code was the first serious attempt to produce a universal code of conduct for doctors and scientists engaged in medical research involving human experimentation. It formed the basis for all subsequent codes, most notably the World Medical Association’s Declaration of Helsinki, first issued in 1964 and revised in 1975. Its central principle is an unequivocal statement of the need for informed consent.
The National Women’s experiment, it appears, violated most articles in the code.
In 1971 Ruth attended the National Women’s colposcopy clinic where the colposcopist, Dr William McIndoe, observed “dramatic changes” in her cervix. The abnormal area visible under the microscope had increased. McIndoe arranged for Ruth’s admission for a cone biopsy which Green performed a month later. The histology report showed microinvasion of the cervix and that the tumour had not been completely removed.
When Ruth returned eight months after the operation for a further colposcopic examination, McIndoe was worried about a small area of unremoved abnormality extending into the vaginal wall and her continuing positive smear. “I would be more satisfied clinically and scientifically)” he wrote, “since this should be quite possible quite safely and readily, to remove this small area which remains.”
Green was out of the country and McIndoe performed the operation himself. The tissue he removed showed carcinoma in situ.
In 1971, for the first time in seven years, Ruth’s next smear was relatively normal with no evidence of malignancy though this would not last. By the end of the year, she was once again showing evidence of malignancy.
Despite this, for some reason, Ruth had no colposcopic examination by Dr McIndoe after 1972.

Women’s. For more than 10 years after he arrived at National Women’s he was the only colposcopist in New Zealand. He trained many practitioners of the new specialty in his clinic. From the time he arrived he worked closely with Associate Professor Herb Green and was the colposcopist for all the women being studied. He was in the position of observing lesions which in any other hospital would have been removed.
Cytologist Dr Stephen Wtlliams describes McIndoe as “professionally very careful, exact and accurate. He was a worrier to some extent, and at times he was in an enormous dilemma about all this business.”
According to a later colleague “He was worried sick about it. He could see people dying and that the standard wisdom being taught was wrong.”
Bill McIndoe is called by those who knew him “very religious”, “a lovely bloke” and ‘”shy”. He died in late 1986, of a heart attack, aged 68.
What can I say to a technician who misses an obviously malignant slide at the screening stage who replies, “What difference does it make anyway, they are not going to take any notice of the result.'”
For 20 rears Bill Mclndoe opposed what he saw happening at the hospital. On June 20, 1966, when Green put forward his proposal to study the natural history of cervical cancer on National Women’s patients, McIndoe objected. At the senior staff meeting he outlined his fears in a memorandum to which he spoke at length: “At our present state of knowledge, rather than swing to an extremely conservative position with respect to treatment, I feel the correct measure would be to aim to remove tissue responsible for the positive smear.” He called Green’s management: “inadequate” both from the point of view of diagnosis and treatment.
However, McIndoe was not a member of the Hospital Medical Committee, the elite group which controlled practices at National Women’s. The HMC was chaired by Professor Bonham and comprised the superintendent, Dr Algar Warren; Green; leaders of the hospital’s clinical teams; the radiologist; and the head pathologist.
Later in the day of June 20, 1966, the HMC approved the Green proposal. McIndoe did not get a chance to express his views at this meeting, views which apparently were supported by at least some of the non-HMC medical staff.
The dangers McIndoe saw were two-fold. First, that by limiting diagnostic biopsies a smouldering invasive cancer could be missed. Second, that by delaying treatment or nor completely removing abnormalities, risks were being taken with women’s lives.
It was an unequal battle. At this stage McIndoe’s was a lone voice. McIndoe is described in his obituary as a “kindly, self-effacing man of complete integrity [who] could not abide sham or hypocrisy in any form. He was a good man whose high principles showed up strongly in his whole life … “
Had he not believed so passionately in the wrongness of the National Women’s experiment, McIndoe would have been content to work behind the scenes, developing the scientific basis of cytology and colposcopy. He had come late to medicine, after training as an electrician, and when he arrived at National Women’s he never quite fitted into the powerful inner group which ran the hospital. It was this unlikely person who challenged Associate Professor Herbert Green.
Almost everybody, supporter or opponent, comes up with similar descriptions of Herb Green. “Domineering”, “belligerent” and a man who could not bear criticisms, are the opinions of his detractors. A member of the non-medical staff who described Green affectionately as a “kind, cuddly teddybear of a man” also talked of his propensity for “getting on his high horse. He was right and everybody else was wrong. He always had the last say.”
McIndoe’s struggle to end the experiment is called by a friend “the battle of his life”. His attempts became more desperate as the tragic scenario he predicted unfolded in the cancer clinic. It was McIndoe who was operating the colposcope, who could see through its powerful magnifying eye the troubling abnormal patches on the cervices of the women he examined. When these women were brought back again and again without the treatment he could see they needed, he could not bear it. Green was the consultant and had responsibility and ultimate control over treatment. McIndoe could not interfere directly in the consultant’s clinical judgement. “I have been powerless to intervene,” he wrote.
Although McIndoe found Green “difficult to cope with”, he persistently challenged him in memoranda and in person. ln 1969 in a long memo he discussed disagreement about specific cases. Later, in 1972, he and Green locked swords on five occasions, once prompting Professor Mont Liggins to interrupt them by asking “Are you two still at it?” McIndoe described these confrontations as “vigorous interrogations”.
The response said McIndoe at the time, was that Green “not only will not, but does not, listen to any comment which does not suit him. I have endeavoured by all means possible in a mature and dignified manner to make my feelings plain…”
Beginning some time in the late sixties McIndoe began keeping a list of patients “who were causing concern”. As the years went on, the lists grew longer.
By March 1971 there had been a death. A full year had elapsed between the date this woman’s punch biopsy had shown CIS and the date she was bought back for a more extensive biopsy which showed invasive cancer. Despite a Wertheim hysterectomy where the internal organ are irradiated before the uterus, ovaries and upper vagina are removed, she died.
“It is very difficult,” McIndoe wrote in a memo, “to maintain a high standard of reporting of the cytology work in such a climate. What can I say to a technician who misses an obviously malignant slide at the screening stage who replies, “What difference does it make anyway, they are not going to take any notice of the result.'”
1n 1971 the National Women’s Hospital Tumour Panel was established with Bill McIndoe as convenor. It is not clear exactly who was responsible for the institution of the panel, but the purpose was to open up to discussion particular cases of gynaecological cancer.
By this stage, Mclndoe had been joined in his campaign by Dr Jock McLean, the chief pathologist at the hospital. Mcindoe’s unhappy role in colposcoping the same untreated women over and over again was matched by McLean’s experience in the subterranean laboratories of National Women’s.
Under the microscope he viewed thin slivers of tissue taken by biopsies and he was aware that he was viewing the same tumours in the same women over and over again. When he reported that the specimens showed CIS, or micro-invasion, or suspected invasive cancer; he was aware these alarming reports were not always acted upon. In other hospitals such reports would have resulted in prompt treatment.
In addition, there had been conflicts between Mclean and Green about diagnoses from pathological specimens. Green would ask for particular slides to be brought to his room where he would sometimes write his own diagnosis beside McLean’s in spite of the fact that he was not a trained pathologist.
McLean calls cancer “an appalling enigma. Even 1.6% of the best treated females will develop another cancer. A woman who has CIS is at risk of developing something nasty. Positive cytology is a red light at a corner. Continuing positive cytology always requires treatment.”
At National Women’s the red light was not always being heeded.
McLean says that junior resident doctors came along to the Tumour Panel meetings to be entertained by hearing Green, McIndoe and McLean slugging it out.
Any staff member could come to these meetings and anyone could introduce cases. As far as McLean was concerned this was “progress”. “It meant controversial cases could be brought out into the open and discussed.
It protected the patients and ensured they could be treated in an orthodox manner. At one point one of the professorial people introduced an amendment that cases could not be introduced by the pathologist, only by clinical people, but it was defeated by a majority of the Hospital Medical Committee.”
The Tumour Panel, however, was not a complete answer. Cases could only be discussed one at a time. It was, says McLean, “like Lord Shaftesbury. We could not get everyone out of the mines at once.”
In 1973 McIndoe decided to take more formal action. Eight years had elapsed since the institution of the study and his attempts to prevent limited treatment of patients had met scant success. He wrote a memorandum to the medical superintendent, Dr Algar Warren, asking for “a reappraisal of policy” for cancer patients. There were women, he said, who because of “limited biopsies” were in danger of having hidden invasive cancer go untreated. He outlined seven cases to illustrate his point.
“More and more ladies were coming back with invasive cancer because of the conservative treatment while Green was going on with his mode of management. Doctors stopped transferring patients and Herb’s reservoir of cases diminished.”
McLean’s accompanying memorandum to the superintendent outlines 14 cases where limited treatment, he said, was “not soundly based”. All the women were eventually shown to have invasive cancer. McLean contented they had probably had it from the beginning but because of inadequate biopsies, it had been missed. “In my opinion,” he concluded, “these patients have had what can be termed varying degrees of delayed and inadequate treatment for a disease that is generally considered to warrant urgent hospital admission for adequate diagnosis and definitive treatment.”
For instance, in one patient’s case, McLean talked about inadequate diagnosis and “excessive delay”. CIS was diagnosed in October 1967, but she received no treatment until six months later when a cone biopsy showed microinvasion with possible invasive cancer nearby. More than two years elapsed before this woman had a Wertheim hysterectomy for invasive cancer of the cervix and vagina.
In another patient the biopsy showed CIS but possibly invasive cancer. No action was taken for a year when another biopsy showed invasion. McLean called this “an example of delay in the definitive diagnosis and treatment through failure to heed the warning of the possibility of invasive cancer in the initial biopsy.”
In his reply, Green insisted that other clinicians were also following his mode of treatment and that other staff were implicated in the policy of limited treatment. He said that by studying the natural history of the disease “a calculated risk that invasive cancer could be over looked” was always present, but he denied that delayed treatment affected survival rates. For early invasive cancers, he said the 10-year survival rate was 96%, so that patients whose cancers were “overlooked or treatment delayed” were not “at a disadvantage”.
He cast aspersions on the quality of colposcopy and pathology and complained that Mclean kept “the best diagnostic slides from many cases in his own private collection under a disease index only” preventing him from having access to them.
He regretted that “Dr Mclndoe’s indecision and doubt could cost a long lead in the elucidation of the problem of the natural history of in situ cancer”.
Dissatisfied with Green’s response, McLean and McIndoe again approached the superintendent with McIndoe listing 100 women whose cases were causing him concern, and McLean concluding with a clear statement of the issues at stake for the women: “When patients are admitted to a public hospital they put themselves in the hands of medical staff with the explicit understanding that they will be provided with at least adequate, and preferably optimal treatment for their complaint. Clinical studies and trials to establish optimal management are at times necessary. However, when in the course of a trial it becomes apparent that patients are at risk, there must be a reappraisal of the trial”.
“Despite what Professor Green may say, the consensus of opinion at present is that any delay in the diagnosis and treatment of invasive carcinoma puts the patient at an increased risk. A survival rate of 96% for Stage 1a carcinoma of the cervix is very good at a statistical level – but not for the four or so women who die from the disease. At our present state of knowledge no one can deny that there is every possibility that with earlier diagnosis and treatment, these four or so patients could be alive.”
By this stage Warren too had become concerned. With him, McLean and McIndoe attempted to take their complaint outside the hospital to the controlling authority. They approached the medical superintendent-in-chief of the hospital board, Fred Moody, who discussed it with the board’s chief executive. Despite the fact that the complaint came from a medical superintendent and two such senior doctors, Moody declined to act.
“The whole thing,” remembers McLean, “was thrown back to the hospital to sort out.”
The Hospital Medical Committee set up an investigation committee of three senior gynaecologists, chaired by Dr Richard Seddon (now professor at Otago Medical School). The resulting response, issued in 1976, vindicated the policy of conservative treatment: “It is the firm opinion of this committee that all staff members involved in the implementation of the policy concerned with this conservative management of carcinoma in situ have acted with personal and professional integrity.”
The 1971 death which had so concerned McIndoe and which and intensified his efforts was put down by the committee to a “colposcopic miss”, the responsibility for which, of course lay with McIndoe.
By this time even Algar Warren who had been initially reluctant to act, was calling the report a “whitewash”.
The unease was spreading, and more doctors were coming to see the validity of McLean and McIndoe’s views. Dr Bruce Grieve, a member of the HMC, supported further investigation and suggested that McIndoe and McLean give reports to the HMC. As time passed, says McLean, ‘”the better was our case. More and more ladies were coming back with invasive cancer because of the conservative treatment while Green was going on with his mode of management. Doctors stopped transferring patients and Herb’s reservoir of cases diminished.”
Despite McLean’s belief that their objectives had been achieved, in all the interviews we conducted in the course of writing this article no one could give us an assurance that the experiment ever ended. It was never formally stopped. No instructions were issued to doctors to abandon practices which by now had been shown to be dangerous.
Dr Gabrielle Collison, who came to the hospital as medical superintendent in
1983, in answer to our questions referred us to Professor Bonham who as chairman of the HMC, then the Ethics Committee, and head of the Post Graduate School throughout this time, had ultimate responsibility.
It is very difficult to discuss the National Women’s Hospital experiment with Bonham because he does not concede that it ever took place. Despite the consensus we encountered with other interviewees that this experiment was to study the natural history of CIS, and despite Green’s documented assertion in paper after paper and in memos which went through Bonham’s hands that that was what he was trying to follow, Bonham insists that the subject of the study was quite different.
We must refer here to a problem we encountered in interviewing Bonham which made clarifying his views difficult. He has a tendency towards circumlocution. Several viewpoints can be contained in the same answer to a question. To take an example: When we asked if in some patients “there had been a deliberate leaving of part of the lesion, the excision of only part of the lesion”, Bonham replied: “No, no, no, not deliberate at all. Not deliberate leaving of it, that sounds, that’s misinterpretation. They were taking enough to biopsy. We could call it a deliberate leaving if you like.”
About one thing Bonham is clear. He insists that the experiment was not to study the natural history of the disease. It was, he says, to study “colposcopic control”, “to treat the patient by minimum interference so long as the colposcopic control was adequate”.
In 1966, he says “it was suggested that it was time we treated people with either less than a hysterectomy or a full cone biopsy. And the offer came from Dr McIndoe that he would be willing to provide colposcopy.”
It was McIndoe’s offer, says Bonham which made the experiment possible. “The theory was at the time that you could adequately follow it [the disease] with colposcopy. That was Mclndoe’s theory.”
It is certainly true that McIndoe did not oppose Green’s plan as strenuously in 1966 as he did a few years later when he could see starkly the reality of its consequences. Nevertheless only a very imaginative interpretation of events could claim that the experiment was to test a theory held by Bill McIndoe.
Where others define colpsocopy as a diagnostic tool, Bonham refers to its use as ”treatment”. Of course, if colposcopy is “treatment” it is not possible to claim that no patient went “untreated”, for all had colposcopic examinations.
McIndoe, says Bonham “could have gone on biopsying until he had taken all the abnormality ”, an absurd proposition, for they were not his patients and he was known to abhor the practice of some clinicians overseas who subjected women to a great number of biopsies without anaesthetic.
In fact, McIndoe objected to his role in the experiment from the start. In 1966 he wrote: “… inadequate tissue diagnosis which can be the only description of the type of biopsy I at present perform (if this is to be the only biopsy done) and follow-up only taking further steps if there is clinical or colposopic evidence of invasion, would seem to me the type of care that should not be followed… If Professor Green’s proposal is accepted I would feel it very difficult to take seriously any cytology reporting or colposcopic assessment.”
Although McIndoe was clearly unhappy about the limited colposcopically directed biopsies Green expected him to do, Bonham still blames him and not Green for the 1971 death of a woman in the study. “I had the notes out on that one… and I am sure that one case that died was a colposcopic miss. I think the biopsies were taken from the wrong part. And I think the person who did that colposcopy is now deceased.”
This version of events not only unfairly blames McIndoe as the colposcopist but ignores the fact that the biopsy showed CIS for which no treatment was undertaken.
Bonham calls the sixties and seventies a “developmental stage” in the treatment of cervical cancer. Although American cancer specialist Ralph Rickhart was of the opinion that the study should never have been started, other cancer specialists said that in the mid-sixties, the proposition was probably acceptable.
There was general agreement, however that by the early seventies, when McIndoe could point to dozens of cases which were causing concern, when a great many women given only limited treatment had returned with invasive cancer and when one woman had died, the study should have been stopped.
Bonham cannot give a date for the time the study stopped. When asked who could have stopped Green’s research, he replied: “I think it would have been stopped jointly by the Hospital Medical Committee at that time.”
Throughout this period Bonham was the head of that committee, and after 1977, of the hospital ethics committee, but he in fact took no action to end the study. The study, he now says, “merged into general treatment. It stopped being a study and became general treatment.”
This was perhaps the most disturbing thing that Professor Bonham said. It puts a question mark over the treatment of all the cervical cancer patients who have attended National Women’s Hospital over the last 20 years.
McLean thinks that ‘”peer pressure forced the study to come gradually to an end”. He is “pretty certain” the limited treatment of women stopped.
McIndoe, however, believed ‘”it never came to an end”. He said that “Green carried on with varied managements to the end of his days”.
In the light of Bonham’s equivocal statement about the fate of the experiment, McIndoe, may well have been right. This view is lent support by what was happening to Ruth in the late 1970s.
After five years of smears suggestive or conclusive for malignancy Ruth was abruptly admitted in 1976 for a ring biopsy: a shallow biopsy removing only the surface cells. All the tissue samples showed CIS and the pathologist reported that “the tumour reached the upper cut edge in several slides”. Despite this report no further action was taken.
Over the next three visits to the hospital clinic, Ruth returned normal smears, reports which a clinician would usually view with scepticism in view of her history.
Ruth was brought back in 1977, but not for treatment of cancer. This time it was because her scarred cervix had stenosed, or narrowed, so that menstruation had become painful. The operation was to stretch open the cervical canal. She was still returning normal smears but the histology report of scrapings of tissue from the inside the uterus showed “fragments of carcinoma… probably in situ”. After her next visit, Green commented on Ruth’s case notes that “the histological report is somewhat surprising”.
Nevertheless, after one more visit he discharged Ruth from the cancer clinic into the care of her general practitioner and gave her a clean bill of health. In his letter to her doctor, he concluded “She has no more chance than the next person of now developing carcinoma of the cervix”.
By the date of her discharge in 1979 Ruth had visited National Women’s Hospital 34 times. She had had 28 cervical smears, five biopsies, four operations under general anaesthetic and 10 colposcopic examinations, but as the final histology clearly showed, she still had cancer.
But this Ruth did not know when she was discharged. “I and my family were delighted. We believed that Professor Green had monitored my condition and that I had never approached any condition that looked like cancer.”

In 1966, the year the cancer experiment officially started at the hospital, Green repeated a test he had heard about overseas. He sent sample biopsy slides to five Auckland pathologists, and in only three cases was their verdict unanimous. Twenty years later he quoted this experience to us in support of his long-term distrust of pathology. “How can you base a theory on such impractical proofs? Tradition demands that the pathologist’s opinion be accepted but he is just as likely to be in error as the clinician. Diagnosis is so uncertain and open to dispute by other pathologists. One man’s cancer is another man’s normality. Countless women have been subjected to unnecessary diagnosis and treatment. I’ve resisted the opinion of the pathologist in many cases. Sometimes I’ve been right and sometimes I’ve been wrong.”
“They want to colposcope everyone now. They want to up-end-all the women in New Zealand. It’s a horrible position for a woman.”
Because he doubted so strongly the accuracy of diagnoses given by pathologists, Green disputes cases which have been identified as progress in invasion. He asks: “Who said they became invasive? I could dispute every one of them.”
When would he accept that there was invasion?
“When you have an obvious ulcerating or fungating lesion,” he replied, “or the woman dies of the disease.”
The year after the experiment started Green wrote that of 503 patients not one had progressed to invasion. The reason for this, he said, was that invasive cancer was ”excluded as far as possible at the outset” of the experiment.
Two years later, Green reported in The International Journal Of Obstetrics And Gynaecology that one case had appeared among the women being studied, but he went on to say that this as to be expected since it was within the normal incidence tor the disease. Another case he predicted would “‘probably appear in 1972”. He postulated that his results differed from overseas reports because of his “insistence on the adequate exclusion of invasive cancer at the outset”.
By 1974 there had been a dramatic change. In a paper in The New Zealand Medical Journal Green called his previous prediction “perhaps over-stated and must be modified, not because of the “rash of invasive cancers (six since 1970) but mainly because of inability of present methods to exclude adequately invasive cancer at the outset.”
This was a profound about-face from his confidence of previous years about the hospital’s thoroughness in excluding invasion. Nevertheless it provided a means of avoiding the more unpleasant conclusion, that his theory was wrong and he had endangered women’s lives.
Green discussed seven cases. In only two does he accept there had been “true” progression and both these had had negative smears after his conservative treatment.
In all five other cases where the danger signal of continuing positive cytology had been ignored, Green reinterprets the evidence. ”From the above case-reports it can be seen that the issue of progression or not to invasive cancer is clouded by inadequate initial exclusion of invasive cancer… and possible overdiagnosis of invasion”. Thus he attributes the apparent invasion to either under or over-diagnosis by pathology. So-called “under-diagnosed” cases could be dropped from the study thus improving the final figures.
The one death he discusses (not included in the seven cases) is blamed on a mistake of colposcopy.
The bold rewrite of events implicates Drs McIndoe and McLean, both of whom were at the time protesting about Green’s actions.
McIndoe was clear about what Green was doing. “He believed that CIS is not a cancer. When it does become cancer, then either it was at the beginning or it isn’t now. He plays with the categories of diagnosis.” McIndoe had more than Green’s seven cases. By the same date, he had compiled a list of 30 cases which were now invasive.
Even if it upset his predictions, Green seemed unperturbed by cases of invasion. He wrote: “It does not seem that it is a very dangerous lesion if only one in 16 incompletely treated lesions progresses to invasion.”
Green virtually ceased publishing after this paper appeared. Ralph Rickart says that “after Dr Green was finally silenced, when he didn’t publish any more or get on the lecture circuit, I didn’t hear anyone doubting that CIS progressed to invasion.”
Green’s explanations about under-and-over diagnosis point to the ultimate folly of the whole experiment. Professor David Skegg of the University of Otago Medical School has been given a concise summary of the problem with what he calls “the unfortunate experiment at National Women’s Hospital”: “Green tries to dismiss the results as being due to either inadequate exclusion of invasion at the outset or over-diagnosis of invasion later. The latter explanation is hardly credible in the case of those women who have died from their disease, and the whole argument betrays circular thinking. If the experiment was incapable of falsifying Green’s hypothesis why was it carried out? Moreover, if invasion could not be excluded confidently at the outset, were the patients warned of the risk that was being taken?”
Why did Green persist in the fact of the increasingly depressing reality in the cancer wards?
Professor Green’s answer would be that he believed what he believed and he needed to convince the rest of the world. As Dr McLean says: “I have no doubt that in his own view Herb was acting in good faith. He believed that CIS was not of any consequence. He felt in his conscience that he was not doing any harm to his patients.”
A member of the administrative staff recalls that Green was very kind to patients in the cancer ward. “He saw young women coming in and dying and he would be very unhappy. He took time and talked so nicely to the husbands and relatives.” Green himself prized his ability to talk to his patients. He remembers with pride how at his retirement the medical superintendent said his patients “think he walks on water “.
Perhaps Green had invested so much in his theory that he was incapable of changing his mind when it became overwhelmingly clear that he was wrong. For 20 years a quote was written on his office blackboard. “Don’t confuse me with facts my mind is made up.”
Cervical cancer had consumed his attention since the mid-1950s. He had written paper after paper on it, had initiated one of the biggest studies in the world; it was the foundation of his career. Had he been right, he would have been a world leader. By the early 1970s he was over 50 and it was too late to carve out a career in a different direction. Already disappointed when, as acting head, he had been passed over as chief of the graduate school in favour of Dennis Bonham, he was never made a full professor.
In 1987 Herb Green still cares deeply about cervical cancer. In his retirement years he has over 2000 cases filed on his computer and spends much time writing papers that are rarely published. Not only does he doubt cytology and pathology, he now rejects other modern technical advances in the management of cervical cancer. He calls colposcopy “the most undignified procedure for a woman”. He hates doing it: “They want to colposcope everyone now. They want to up-end-all the women in New Zealand. It’s a horrible position for a woman.” Of the recently introduced laser which allows less destructive treatment he says” “It’s a toy, a gimmick.”
Underlying his attempts to prove his theories there seems to be a kind of fatalism about life and a medical nihilism. He sees a need to accept the inevitability of suffering and death. “We’ve got to accept cancer,” he says “Cancer in our culture has become a dirty disease. We must cut it out, burn it, abolish it. We are asking for prolonged life.”
Professor Green was not the only player in the tragedy which unfolded at National Women’s. But from the professor down, no one but McLean and McIndoe would take him on. As McLean said: “For many years I felt isolated. I kept away from the clinicians. I felt an antipathy against me. They feared I would open my mouth too wide. They have spoken behind Herb’s back, but they won’t confront him. Have you tried arguing with him? Herb’s an absolute bastard when stood up to. People were frightened of him. When McIndoe and I tried to stand up to him Green reacted by doing nothing and saying nothing. He’s a bigoted zealot. He’s like a missionary who thinks he can do no wrong.”
Another scientist said: “I learnt early you produced data and didn’t discuss it. There was no point in talking to him. You couldn’t discuss scientific validity.”
McIndoe added: “It wasn’t possible to get the medical profession to take this fellow on. He had a Muldoon personality.”
Professor Bonham views the struggle between McIndoe and Green as merely a personality clash. “McIndoe and Professor Green didn’t get on terribly well together… if there had been greater harmony among individuals involved in this group things might have happened a little sooner… Bill McIndoe was a charming chap, but he did have a vicious streak. Which made it very difficult – you can’t talk about this really: about someone who has died but it made it difficult.”
Professor Bonham believes that “in an academic scene you need a few free thinking people to stimulate in various directions… Herb Green was a unique sort of free-thinker. I had to live with him for a lot of my life. Though it was sometimes difficult because of his fairly free ideas, he fitted into the department extremely well and we didn’t have problems. No one would be unhappy with the way he managed the patients with cancer. He really looked after them fantastically.”
When Ruth noticed slight bleeding between her periods two years ago she was not unduly worried. “I was approaching 49 and thought this could merely indicate the onset of menopause. When I visited my doctor about a painful shoulder, I suggested that I should have a smear test, as I had not had one since leaving National Women’s at the end of 1979.”
Her latest smear was suggestive but not conclusive for malignancy and she was referred to a specialist. “I took the liberty of reading the referral letter before the appointment. On reading it my husband and I were alarmed that it mentioned carcinoma in situ. We looked up this term in a medical dictionary and were disturbed to realise that I had been seen for a condition which without treatment could lead to a truly malignant cancer.”
The specialist told Ruth that her National Women’s Hospital records revealed that her earlier smears had shown carcinoma in situ. She had in effect, “been sitting on a time bomb”.
The biopsy he performed showed that Ruth had invasive cancer.
“I was now facing the reality of cancer. I felt that angry and frustrated. First, Professor Green had never informed me of my condition over the years, nor did I feel that my treatment from 1964-79 had been satisfactory. I had had a ring biopsy performed on me in 1976 when I was 40 years of age. I could not see the point of continuing with biopsy treatment at that age. I had not had a child since 1966 and had no intention of starting another pregnancy in 1976 when my career as a secondary school teacher was well underway. At no time had I been fully informed or given any say in the treatment I received.”
In October 1985, Ruth entered National Women’s Hospital. For two days she lay behind lead shields with caesium rods inserted into her cervix. Six weeks later she returned for surgical removal of the uterus, tubes and ovaries. She spent New Year’s Eve in hospital and was discharged in January 1986.
The authors had gone back to the tissue samples and smear tests for all the women who had been diagnosed as having CIS at the hospital since 1955. The raw data for the 948 women was analysed, making it the largest study of its type in the world. The study divided the women into two groups – 817 who had normal smears after treatment by “conventional techniques” and a second group of 131 women who had continued to produce persistent abnormal smears. This second group is called in the study the “conservative” treatment group. Some had only biopsies to establish the presence of disease and no further treatments. Others had abnormal smears after initial treatment and were not treated further. For example, one woman had 22 malignant smears over 16 years after hysterectomy, but no further treatment. She eventually developed invasive cancer of the vaginal vault.
A most significant finding was that in only 5% of the group-two “conservative” treatment patients did CIS disappear. That is, 95% continued to have CIS, or worse. Twenty-nine, or 22% of these women, developed invasive cancer of the cervix or vagina.
“They went through all my personal files from the hospital and from my GP. I can only liken it to a rape case. I felt so exposed and vulnerable.”
In contrast, the group-one patients who had normal cytology after treatment rarely developed invasion. Only twelve, or 1.2%, progressed into invasion.
Such enormous differences in outcome demonstrated beyond the shadow of doubt that women with continuing abnormalities ran a very high risk of developing invasive cancer.
Twelve of the total number of women had died from invasive carcinoma as had four, or 0.5%, of the group-one women, and eight, or 6%, of the group two women who had limited or no treatment.
There is one small group of women in the study which deserved special attention. Twenty-five women had only a diagnostic punch or wedge biopsy and no further treatment, 18 of this number only ever having a had a single biopsy “with minimal disturbance of the lesion”. These were the women who could most clearly show “the natural history” of CIS.
Ten of these 25 women who only had diagnostic biopsies developed invasive cancer. Worse, almost all of the women who had continuing abnormal smears after the biopsy developed invasive cancer. There were 10 women in this group, and nine of them developed invasion.
The authors concluded the study by saying that “it is, therefore, impossible to escape the conclusion that patients with continuing abnormal cytology… run an unacceptably high risk of developing invasive carcinoma compared with women with continuing normal cytology.”
The women with abnormal cytology, that is, the group-two women, had an “18% chance of developing invasive carcinoma of the cervix or vaginal vault at 10 years, and a 36% chance at 20 years.” The study had clearly shown that “CIS of the cervix had a significant invasive potential”.
Green’s thesis that CIS was a harmless lesion, and invasive cancer a separate disease, had been disproved by his own data.
When interviewed, Green disputed the findings of this study on the basis that the pathology was incorrect. He could not accept that all the invasive cases were really invasive.
On three occasions during our interview with him, Green raised the subject of the deaths of the women. Unasked, he said: “It’s unfair to accuse me of studies which lead to deaths, when they were part of it.”
“But we haven’t said that to you,” we replied. “Who has?”
Eight of the 131 group-two women died. If the death rate in this group had been the same as the group-one women, none would have died.
Scientific method depends on the publication of results which disprove as well as those which prove a hypothesis, but Green never completed his study or published the final result himself.
McIndoe and McLean decided to work on and publish the study because they wanted to bring what had happened out into the open. It was drafted and redrafted over several years and statistician Mullins was brought in “to provide a stronger statistical basis for making the statement. They wanted to nail it down more firmly.”
“We tried to make it impersonal,” says Mullins, “so we couldn’t be accused of a witch-hunt. The ethical issues were drawn and highlighted.” Green’s name is not mentioned in it.
McLean had given some of the data at an international pathology conference in Sydney in 1982: “I got very good feedback from the top gynaecological pathologists in this field. One of the top gynaecologists in the UK came to me afterwards and the first word he said was ‘litigation’. He thought there would be some. Because of the efforts on the part of some staff here to sweep the thing under the table we wanted to bring it out into the open and let our peers judge. They’d tried to cover it up and shut me up. The finding vindicated us.
“We didn’t make it too public in the hospital that we were working on it at first, but in general the clinical staff were supportive. They were too frightened to stand up themselves, but were quite happy to let someone else stick their necks out. It’s like penguins on an ice floe. They push one in first, and if he doesn’t get eaten by the killer whales, they all jump in.”
The authors of the study hoped the academic media would pick it up and were disconcerted when it didn’t, as Mullins puts it, “make more of a splash”. “There were some reprint requests from overseas”, he says, “but none from New Zealand.” If overseas doctors saw the issues, it was not so clear to the New Zealand medical fraternity.
Although he agreed that in general scientific findings should be published, Bonham was critical of the paper. “They were unethically describing Green’s cases to some extent and poking the finger a bit at him. There are innuendoes in that paper that shouldn’t be there.”
Bonham had outlined his concerns in a letter to the medical superintendent in November 1982 before the publication of the study: “I have heard a rumour that Dr McIndoe and possibly another specialist, have being reviewing case of carcinoma in situ that have been managed in the hospital. I have no recollection of approval being given for review of in situ cases belonging to other consultants, and I wonder if they have been reviewing cases by courtesy of Miss Owen (the secretary of the clinic) without the approval of the clinicians concerned.
“This may only be a rumour, but I think it may be worthwhile your having a look at it in the first instance because any publication emanating from this hospital must be acceptable to the staff of the hospital before it is submitted for publication, as I am sure you will agree.”
Mullins said the McIndoe was motivated most to write the paper by concern for the future if Green’s attitudes continued to have influence. “He thought Herb Green’s theories would fade away and Dennis Bonham would change his mind.”
A friend of McIndoe’s told us that he “went through the agonies over writing the paper. He didn’t think anything would be served by pillorying Green, but he worried about the future, particularly about the effect on doctors trained at National Women’s who would not keep up with the research. Green’s teaching was still being followed out there amongst the GPs.”
While Ruth was visiting her specialist before her hysterectomy, he had mentioned that her National Women’s Hospital records showed that she had had a cervical smear in 1982. “This threw me a little,” remembers Ruth, for she was quite sure that she had not had another smear test after being discharged from the hospital in 1979.
When Ruth was admitted for her operation, the house surgeon also mentioned that the hospital had received smear reports from her GP. “I told him that I would like to see one of those reports. He passed me my file. On it I saw clearly in print on two occasions “Alive and well – with evidence of cancer.” I asked how in the hell my GP could say that when he was not doing smear tests”.
The house surgeon told Ruth that her GP should have been performing a smear test annually. This he had not done. What he had done, however, was fill in the hospital cancer clinic follow-up forms as if he had, and return them to the hospital. This he did in 1980, 1982 and 1984. He even provided dates when the non-existent smears had taken place.
When Ruth realised the full enormity of the mismanagement of her case she decided to take some action. She had the choice of proving medical misadventure through the Accident Compensation Corporation and thus recouping some of her sick leave or taking a case against her GP to the Medical Disciplinary Committee. “I had to decide between ACC, which would have been good for me personally, or protecting other women by exposing my doctor.” Ruth decided on the latter course.
Ruth describes the disciplinary hearing as a harrowing experience. The hearing was conducted like a trial with lawyers, people sworn under oath and cross-examination. A panel of five men, three doctors, a legal assessor and an ex-serviceman, would make the decision. The hearing lasted from 10am till 3.45pm. Ruth was cross-examined in the witness box for “what felt like 24 hours. The lawyer tried to put words in my mouth. His main thing was that at National Women’s I would have been told I should have follow-up smear tests. I got to the stage I thought I couldn’t take any more. Then, thank God, he stopped.”
Apart from her lawyer, Ruth had no support in the courtroom. “They went through all my personal files from the hospital and from my GP. I can only liken it to a rape case. I felt so exposed and vulnerable.”
Ruth’s lawyer called a National Women’s Hospital cervical cancer specialist, Dr Murray Jamieson, to question him about the hospital’s handling of Ruth’s case. The committee also wanted to know why the hospital had not acted on the GP’s report of continuing cancer. Jamieson replied that many doctors filled the forms in improperly, and anyway, it was assumed that if there was evidence of continuing cancer, the doctor should have done something about it. Responsibility then was laid at the door of the GP.
Four weeks after the hearing Ruth’s lawyer received the committee’s written decision. Her GP was found guilty of professional misconduct and censured, but in mitigation the committee noted that Ruth had not asked for a smear after being discharged and said that her doctor had been “influenced by the over-optimistic opinion” of the National Women’s specialist. The GP was ordered to pay the court costs of $1551 of Ruth’s legal expenses. This left her with a bill of $1500 for legal fees.
She did not have the satisfaction of helping other women because the committee also ordered that there should be no publication of the doctor’s name in the New Zealand Medical Journal and no publication of details of the findings “in such a way as to identify either the complainant or the doctor” in any other media. For this reason we have been unable to use Ruth’s real name in this article.
“I felt the whole thing had been a bit contradictory. In no other court in the land does a person found guilty have their name suppressed without a very good reason. Why should doctors be immune from the normal laws of society?”
They say “… some southern authorities have promised New Zealand an epidemic of that disease. Every woman should be screened. We are told that cervical cancer is a sexually-transmitted disease. True, the victims are not eaten by worms, but gnawed away by cancer (or fear of it). The wages of sex is a positive smear.”
On the surface this further sad chapter in the mismanagement of Ruth’s illness could be seen as just bad luck. Perhaps Ruth was unfortunate to be under the care of a sloppy GP. There is another more likely explanation.
The attitude of Ruth’s GP suggests the whole climate of training about cervical cancer has been affected. Ruth’s GP had done his post-graduate training at National Women’s Hospital in 1976. Consequently he may have felt justified in not taking further smears if he had been taught that smears were inaccurate, of limited value and cervical cancer relatively unimportant. Especially when he read the letter of referral from Green which said that Ruth had no more risk of developing invasive cancer than the next woman. It seems that Green’s attitude has spilled over into a negative, sceptical attitude to cervical cancer screening among doctors.
The investigation for this article met with great discouragement from doctors. With one or two exceptions, they said to leave it alone, it was in the past and no good would be served by revelations in the lay media. It was seen as a matter for the medical profession, not the public. Most doctors refused to talk at all; others were encouraging, but declined to be quoted.
However, cancer experts overseas were more forthcoming in their opinions. Most knew about “the unfortunate experiment” at National Women’s. It was not necessary to explain to any doctors, local or overseas, what the experiment had been about. Yet whatever their personal views, the New Zealand medical profession closed ranks to protect the reputation of their fraternity.
The unfortunate experiment is not an issue of the past. It has continuing repercussions for the women who were part of it, who have to live with cancer now or in the future. But it also has implications for the treatment of cervical cancer today, and for the future of New Zealand’s long overdue cervical cancer screening programme.
The cervical cancer rate has dropped in countries that have a programme of screening women by systematically taking cervical smears, but in New Zealand which has no population screening programme, the number of cases has not declined. The rate of deaths from cervical cancer is gradually increasing, and some doctors talk about an alarming “epidemic” of the cancer among younger women who rarely showed cancer in the past
Many women in New Zealand do have cervical smears taken by general practitioners, family planning clinic doctors or during ante-natal care, but the coverage is haphazard and the groups most at risk are the least likely to have regular smears. Of 40 cases of invasive cancer at Wellington Women’s Hospital in 1986, 14 had had a previously abnormal smear which had been ignored. Others had been treated for gynaecological problems but had not been given a smear test, while several women had asked for an examination and been refused.
New Zealand lags behind the rest of the world in every area of the management of cervical cancer. Some of the country’s major diagnostic laboratories still use outmoded Papanicoloau grading system which has been abandoned in more advanced parts of the world. The care of women with cervical abnormalities is haphazard and casual. Women are brought back endlessly for repeat smears when they should be referred for colposcopy. There are under 20 colposcopes in the country where there should be twice that number. Consequently, at Middlemore Hospital “older” women are not referred for colposcopy after an abnormal smear but proceed straight to a “blind” cone biopsy, a practice frowned on by cancer experts. There are only two lasers, the treatment technique that is the least damaging in many cases.
National Women’s is the primary teaching hospital in gynaecology. It controls undergraduate teaching in gynaecology at the Auckland Medical School and is the home of the Post Graduate School of Obstetrics and Gynaecology where doctors are trained in the speciality.
Professor Green controlled the teaching on cervical cancer until he retired in 1982. In his view “screening is the biggest hoax ever perpetrated on New Zealand women”. He thinks cervical smear tests for screening are a waste of time and money. He contends that more women will die from hysterectomies because of false negatives than if they had been left to die of cervical cancer.
The only way to prevent cervical cancer he says would be to stop “fornication”.
When we asked how you would detect CIS before it became invasive without screening, he replied” “You won’t. All you can do is reduce the effects [of invasive cancer] by early diagnosis.”
He emphasises the importance of history taking, asking women about any unusual bleeding or discharge which can be signs of invasive cancer. These symptoms, however usually only appear once the cancer is invasive and the woman’s prognosis worse than if the cancer had been detected at an earlier stage.
Green believes there are “vested interests” in the current push to set up a nationwide screening programme for women. There are academic careers to be built, he maintains, and talks of the “colposcopic empire” – gynaecologists motivated by the prospect of a great increase in expensive colposcopoic examinations.
This contention is contradicted by the fact that most colposcopes in New Zealand are in public hospitals where no private financial interests are involved. Twenty colposcopes hardly constitute an empire.
Green is undismayed that his views are regarded as idiosyncratic outside National Women’s Hospital.
Green’s successor as teacher and head of the cervical cancer team at National Women’s is Dr Murray Jamieson. The son of a non-conformist minister, Jamieson became a Rhodes Scholar before going as a surgeon to Vietnam after a stint in the territorials. Later he became Green’s registrar at National Women’s.
Jamieson is one of the new generation of “baby boom” doctors. Many believe that he is being groomed by Professor Bonham to be his replacement when he retires.
At his invitation we attended one of Jamieson’s lectures on cervical cancer. It was impeccable and taught the generally-accepted position on cervical cancer screening. Jamieson said he had always taught this way. However, two years ago the head of one of the hospital’s other clinical teams was so disturbed at one of Jamieson’s lectures that he stood up and presented an alternative pro-screening view.
Like Professor Green, Jamieson prefers early diagnosis of invasive cancer to prevention by screen. There is an 80% cure rate for invasive cancer, he says, “a great deal higher than any other cancer”. The other way of looking at this, of course, is that at least one in five women with invasive cancer will die, women who might have been saved by earlier treatment.
In August 1985 Jamieson and Petr Skrabanek, a Hungarian working at the University of Dublin, published at letter in The New Zealand Medical Journal entitled Eaten By Worms: A Comment on Cervical Screening in which they quote classical and Biblical beliefs that sexual misconduct was the cause of genital cancer. They say “… some southern authorities have promised New Zealand an epidemic of that disease. Every woman should be screened. We are told that cervical cancer is a sexually-transmitted disease. True, the victims are not eaten by worms, but gnawed away by cancer (or fear of it). The wages of sex is a positive smear.
“In the 30 years from 1953 to 1982 no more than an average of 90 women a year have died of cervical cancer, compared with almost 2000 persons who died in 1982 from accidents, poisoning and drowning, or to the 34 suicides and 41 homicides in that year.”
The letter concludes that screening is therefore hardly worth the considerable effort involved. “Why then do we fuss so much about cervical cancer? Every woman should have smear, correct? Every woman should be reminded there is a danger? Why? Is it because the fear of being eaten by worms is a healthy fear? Should one million New Zealand women over the age of 19 live in daily fear, though only 0.009% of them will enter the final statistics? Listening to and asking leading questions of patients is far, far better than screening in the control of cervical cancer.”
Dr Jamieson says this letter is not evidence that he is opposed to screening. He dismissed it as a joke. Intended as a lampoon.
Professor Green describes himself and Jamieson as particularly “close’.
Today Dr Gabrielle Collison, National Women’s medical superintendent talks of “two camps” in the hospital, a “pro” and an “anti-screening camp”. Professor Green says the pro group consists of the part-time clinicians; the anti group of the professorial school.
However, Professor Bonham insists that doctors who see National Women’s as anti-screening have all been reading “bunkum from Skragg” (sic) whose views he calls “false and libellous”.
Professor David Skegg, an epidemiologist from Otago Medical School, has been one of a number of doctors not connected to National Women’s who have been trying to persuade medical opinion of the need for a screening programme. He is the author of the Skegg Report, published in The New Zealand Medical Journal in 1985, which reviewed the evidence for the effectiveness of screening and provided a model for a possible programme in New Zealand.
While in many countries such a programme might not be necessary, says Skegg, in New Zealand it was “because National Women’s Hospital, which is very influential, has over about 15 years contained some people who have been very anti-cervical screening, and I think it would be impossible to overestimate the effect that has had on medical training.”
Other New Zealand doctors talk about the National Women’s “party line”. Dr Ian St George, a lecturer in general practice at Otago Medical School, said that through National Women’s role as a teaching hospital Green’s theories have had a “profound influence” both on practice and on the lack of screening in New Zealand. If doctors were to be educated about the value of screening, he says, it would be necessary to “address the issue of Herb Green and the influence his teaching has had in New Zealand, and show that it was wrong; there are still plenty of people who rationalise their lack of effort in taking cervical smears on that opinion”.
Dr Allan Gray, medical director of the Cancer Society of New Zealand put it more strongly. “They are totally up a gum tree. It’s like belonging to a political party. Teaching at National Women’s is not authoritative on this issue. It’s a big disaster area. All the teaching at one medical school is totally out-of-date and incorrect. They’ve taught several generations of doctors the wrong thing. A lot of practitioners won’t do smears because they don’t believe in them. They have been taught that it’s useless.”
It is clear, then, that National Women’s Hospital is a crucial factor in the success of any nationwide cervical screening programme. But no one has been prepared to directly confront its power. Even doctors who want screening avoid rather than confront the problem at National Women’s Hospital.
The cervical cancer symposium held at Auckland Medical School in 1986 was organised specifically to counteract the National Women’s Hospital influence. “The Cancer Society,” says Allan Gray, “paid for the two overseas speakers in the hope of bringing in a glimmering of light.”
No one was prepared to publicly confront Professor Green about “the unfortunate experiment” at National Women’s. He retired with his career intact. A eulogy written by his colleague Professor Liggins in the Auckland University News only praised Green. “His views which were condemned in the 60s as revolutionary and dangerous were largely vindicated in the 70s to the extent that as he retires he has the satisfaction of seeing worldwide acceptance of his conservative approach.”
The silence stems from the medical profession’s rigidly-enforced loyalty among its members. Doubtless the doctors who did talk will be condemned by some of their brethren for breaking ranks.
Ruth’s lawyer encountered that same silence when he tried to find a doctor who would testify to normal handling of a case like hers. He was refused by several doctors.
Professional solidarity is always a priority for the medical profession because it is basic to their power. There are many penalties for those who violate the code. Such doctors are marginalised and their careers stalled.
Covered by his medical insurance, Ruth’s doctor only suffered a day’s embarrassment for his life-threatening negligence. Had his crime been against the profession and not the patient, he might well have suffered a more severe outcome.
The right of the doctor to treat his patient as he wishes is absolute. For over 20 years, no one interfered in Professor Green’s treatment of patients. Eventually, new cases were not referred to him, but no one intervened on behalf of the women he was already handling. In the medical system, there is no voice for the public interest.
With no public scrutiny, regulation is supposed to come from peer review, that is, evaluation by others in the trade.
Some doctors say that such a situation as happened at National Women’s could not recur because peer review is now so widely practised. “The bad old days of the consultant as a tyrant are gone,” Dr Collison told us. Most hospitals now have ethics committees to monitor practices.
But ethics committees are invariably dominated by doctors, and all members are appointed by the hospital with Hospital Board approval. They are not publicly elected. At National Women’s Hospital the ethics committee consists of doctors, one nursing and one lay member. It is chaired by Professor Bonham. Although the committee was instituted in 1977, it appears it failed to investigate or definitively terminate the experiment begun in 1966.
Autonomy is crucial to the power of the profession. Doctors are fanatically jealous of any encroachment on this autonomy. The profession is entirely self-regulating and beyond scrutiny. Doctors are accountable to no one but each other. To preserve this autonomy, the public must learn as little as possible about medical bungles. Left to them the story of the “unfortunate experiment” would have been buried with the victims.
This article was first published in Metro in June 1987.